One of the most common pathologies of the musculoskeletal system is osteoarthropathy of the hip. The progressive process affects hyaline cartilage, destroying bone and connective tissue. One mobile connection and both are affected. The second name for the condition is hip joint disease, which is more common in women after the age of 40.
cause of disease development
The disease is not hereditary, but the presence of genetic traits in the tissues and bones can motivate its development and transmission from parent to child. Hip disease is considered an age-related problem, which is caused by the aging of the body. In some cases, the destructive process of the hip joint begins in young people.
The main causes of hip arthrosis include the pathology that causes the pathological process:
- tissue damage (femoral neck fractures, contusions);
- Vigorous physical activity (exercise, weightlifting);
- joint infection (arthritis);
- femoral head necrosis;
- obesity;
- Endocrine diseases, such as diabetes, metabolic disorders;
- Scoliosis.
The hip joint is destroyed under the influence of various factors. Thus, people with a genetic predisposition, who are overweight, who have heart disease are at risk.
disease type

There are two types of arthrosis of the hip:
- Primary or idiopathic. 50 years later development. The difference lies in the symmetrical lesions of the joints. The procedure was disappointing and it was difficult to determine the cause of the destruction of the pelvic joints.
- middle school. It is characteristic of youth, driven by various pathologies. The failure of one joint is characteristic: left or right. The process is slow, and if you take the medicines prescribed by your doctor and follow the recommendations, the pathology responds well to treatment.
This disease causes the complete destruction of the joint.
Degree and characteristic symptoms of hip arthrosis
The destructive process of the hip joint occurs gradually, and each of the three stages is accompanied by unique symptoms:
- early days. Arthropathy of the hip joint grade 1 with signs:
- Intermittent hip pain caused by exercise, pelvic pressure;
- groin discomfort;
- no movement restrictions;
- The joint space is slightly narrowed.

- secondary illness. There is deterioration in the pelvic region with localized temperature rise. Pain at rest and with exercise. The development of 2nd degree arthrosis of the hip is accompanied by the following symptoms:
- The pain syndrome is intrusive and intense, especially at night;
- A characteristic "starting" pain with movement after rest;
- limited movement, leading to cartilage destruction and inflammation;
- limp appearance;
- Difficulty abducting the foot and bending the limbs;
- muscle wasting, and the affected leg looks flabby;
- The joint space is narrowed, and there is bone compaction during angiography.
- Finally, stage 3. She spoke of irreversible processes. It is accompanied by the following symptoms:
- joint injuries and general deterioration of the condition;
- Changes in the size of the lower extremities;
- limp when walking;
- Joints do not move at all, which blocks the pelvic joints;
- Lack of cartilage layer, bony surface connected.
Diagnosis of joint disease

The appearance of early symptoms does not force a person to go to a clinic, he prefers self-treatment. Arthropathy of the hip joint, however, requires urgent medical attention and prompt diagnosis. In consultation, the presence of arthritis leading to complications in the form of hip arthrosis was refuted or confirmed. To do this, turn to the following experts:
- therapist;
- neurologist;
- rheumatologist;
- Orthopedic surgeon (surgeon).
The examination is complex, therefore, all diagnostic measures are carried out in two directions:
- clinical diagnosis:
- Inspect (to find out where the injury is);
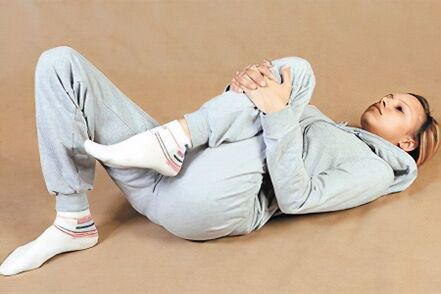
- Limb flexion, extension, rotation;
- Asymmetrical legs;
- Pain on palpation.
- Instrument check:
- Radiography:
- CT;
- nuclear magnetic resonance;
- ultrasound;
- Aspirate fluid from the joint cavity (if necessary).
What treatment is needed?

The goal of all treatment procedures is to reduce pain and improve joint mobility. Hip disease can be treated in a variety of ways, depending on the extent of the injury.
Conservative treatment is adopted in the early stage of development, pathological development is stopped in the second stage, and 3rd degree arthropathies can be cured by radical methods.
After confirming the diagnosis of hip arthrosis, a doctor prescribes a package of treatment measures, including medication and a physical therapy program. Treatment is aimed at eliminating the symptoms of pain and inflammation, stopping these processes. In severe cases, prosthetic surgery is used.
conservative approach
For hip arthrosis 1st and 2nd degree, a comprehensive approach can help: medication, therapeutic massage, gymnastics, osteopathy. Treating joint disease non-surgically means avoiding surgical intervention. First, your doctor will prescribe pain medication to relieve the painful symptoms that persist with grade 2 hip arthrosis.
drug
Drug therapy includes the use of the drugs listed in the table:
| group | Therapeutic effect |
|---|---|
| Anti-inflammatory (non-steroidal) | Symptomatic, helps anesthetize limbs, has anti-inflammatory effect |
| Steroids | They are used to help relieve pain and inflammation when non-steroidal medicines have not worked. |
| Chondroprotectant | Restore cartilage tissue structure and improve synovial fluid production |
| hyaluronic acid | Inject into joints to lubricate articular surfaces |
| muscle relaxant | Reduce muscle tension, improve blood flow in blood vessels |
physiotherapy
For hip disease, massage, exercise therapy, electrophoresis, cryotherapy, and many other treatments are useful. Let's take a closer look at the main ones:
- Exercise therapy is the basis of treatment. It will help localize the disease in any part of the body. A special exercise system will strengthen muscles and eliminate discomfort during exercise.
- Massage and manual therapy - passive recovery of muscles. Especially useful in the first stages of pathological development.
- Phonophoresis uses ultrasound to enhance the effects of medicines. If the TBS area is smeared with medication and ultrasound is applied, it penetrates the skin quickly.
- Joint traction. Using special instruments increases the joint space.
- diet. Helps reduce joint stress. Properly chosen products improve well-being, but dietary nutrition is not included in the main treatment.
folk remedies

At home, traditional medicine approaches come to the rescue. The patient may be warmed up and applied with compresses to reduce inflammation and swelling.
Applying compresses containing honey, aloe vera juice, and sea salt can help improve blood circulation in the inflamed area by providing plenty of blood to the inflamed area. Folk remedies are part of the initial complex treatment, as well as for grade 2-3 pathology.
Severe injuries require surgery. Diseased joints are replaced by metal joints.
Prevent Hip Disease
Preventing hip disease is not difficult. You must follow the recommendations below:
- exclude a sedentary lifestyle;
- do excercise;
- monitor weight;
- reject bad habits;
- Timely correction of congenital and acquired defects of the hip joint.
Hip disease is dangerous, so prevention after 40 years is very important for everyone. But there is also a risk group that includes athletes and people with a genetic predisposition. When symptoms like this occur, be sure to seek medical attention immediately. Early diagnosis will allow you to get effective treatment and avoid surgery.





































